| « COVID: If they haven’t isolated the virus, how can they make a vaccine? | David Rasnick: new strain of the coronavirus, or a giant con? How deep do the lies go? » |
Your Coronavirus PCR Test is Positive – You Still Might Not Have Covid-19, Exposing Unwelcome Truths About the Deep Flaws of PCR Testing
Preface by Gary G. Kohls, MD
New York’s state lab has access to the Cycle Threshold (Ct) values from the PCR tests they process. Last July, the lab identified 872 positive tests based on a threshold of 40 cycles.
If the lab has used a cutoff of 35 cycles, 43 percent of those tests would have been considered negative. What’s more, if the cycles had been limited to 30, 63 % of the PCR-positive patients would have been justifiably been regarded as negative.
In testing data that include cycle thresholds, officials in Massachusetts, New York and Nevada have found that up to 90 percent of people testing positive carried barely any virus. If that data was extrapolated to nation-wide statistics, the 45,000 new “cases” reported last week perhaps only 4,500 would actually need to isolate and submit to contact tracing
It is obvious that PCR tests need to be interpreted with caution as they do not reflect a true viral load, infectivity or even contagiousness. In fact, many times no viable viruses can be cultured in patients with a positive PCR test result. False positive PCR tests abound, resulting in CDC statistics that have been consistently over-estimating both the incidence rates and mortality rates related to the current epidemic, thus falsely stimulating the panic seen among the many people demanding their vaccinations NOW.
Studies in France, Canada and Singapore, as reported in the August 25, 2020 issue of Clinical Infectious Diseases, have tried to culture the Covid-19 virus in patients that had positive PCR test results when the number of “cycles” used in the test exceeded 30. The scientists doing the studies were unable to culture any virus in those patients. Since many PCR test kits in the United States use cycle thresholds that are actually greater than 35, there is a serious problem with the PCR test, which is considered the “gold standard” for diagnosing SARS CoV-2.
In view of the general consensus (including recent acknowledgements from both the WHO and CDC) that PCR cycle thresholds (Ct) above 30 results in increasingly large false positive test rates that approach 100%. (Note that 30 cycles represents a million replications of the RNA particles and 40 cycles represents a trillion replications.)
If it takes a trillion multiplications of a test before any viral RNA fragments (much less viable viruses) can be identified, you can be sure there are not enough viral particles to cause a disease.
Below is some information that should help people understand why mRNA vaccine hesitancy makes total sense.
PCR cycle threshold (11-37) and positive cell culture (black line, 100% to 0%). The colored bars indicate the number of positive cell cultures per Ct per week after infection (1 to 3 weeks). (Jafaar/Raoult)
The above chart is from a French research group that has recently shown that at a cycle threshold (Ct) of 25, about 70% of nasopharyngeal samples were viral culture positive (i.e. were infectious). At a Ct of 30, only 20% of the samples were culture positive. And at a Ct of 35, a miniscule 3% of samples remained culture positive. Above 35, all samples were negative. This means that if a person gets a “positive” PCR test result at a cycle threshold of 35 or higher (as applied in most US labs and many European labs), the chance that the person is infectious is less than 3%. The chance that the person received a “false positive” result is 97% or higher. The chart above correlates PCR test positivity (black line) with culture results for the tested-for virus (colored bars). If more than 30 cycles are required to get a PCR-positive test result, the cultures will be consistently negative/sterile, meaning that any positive PCR test that only becomes positive after 30 cycles can be called a false positive.
Many PCR test kits on the market use a PCR Ct that is actually above a useless 35! Those kits will naturally result in large numbers of false positives that have already corrupting the CDC’s and Department of Health’s Covid-19 statistics – and also the CDC’s drive to get people inoculated as rapidly as possible with the experimental - and untested for long-term safety and efficacy – the two mRNA vaccines. It is therefore imperative for patients who take a PCR test to know what test kit brands are being used (see partial list below) in your hospital or Public Health Dept laboratory.
Here is a helpful quote: “…if a person gets a ‘positive’ PCR test result at a cycle threshold (Ct) of 35 or higher (as applied in most US labs and many European labs), the chance that the person is infectious isless than 3%. The chance that the person received a “false positive” result is 97% or higher.” – Swiss Policy Research
So, if someone has typical flu symptoms or an influenza-like-illness (ILI) and a positive PCR test that might be a false positive (ie, one that only turns positive at a cycle threshold over 30), perhaps your disease is something other than Covid-19 and shouldn’t be reported to the CDC as Covid-19. Something to think about.
Quest: 50 cycles
Inbios: 45 cycles
Luminex: 45 cycles
Gnomegen: 39 cycles
ThermoFisher: 37 cycles
Read on for much more from some powerful investigational journalism done by New York Times journalist, Apoorva Mandavilli.
________________________________
Your Coronavirus PCR Test is Positive. Maybe it Shouldn’t Be
The Usual PCR Diagnostic Tests May Simply Be Too Sensitive and Too Slow to Contain the Spread of the Virus
PCR Tests Authorized by the FDA Provide Only a Yes/No Answer to Covid-19 Infection but Will Still Identify as Positive Even with Low or Zero Amounts of Virus in Their Bodies
By Apoorva Mandavilli - Published August 29, 2020, Updated Sept. 17, 2020 (2068 words)
https://www.nytimes.com/by/apoorva-mandavilli
“This number of amplification cycles needed to find the virus (or small fragments of the virus’ DNA), called the cycle threshold (Ct), is never included in the results sent to doctors and coronavirus patients, although it could tell them how infectious the patients are”
“In three sets of testing data that include cycle thresholds, compiled by officials in Massachusetts, New York and Nevada, up to 90 percent of people testing positive carried barely any virus.”
“Officials at the Wadsworth Center, New York’s state lab… identified 872 positive tests, based on a threshold of 40 cycles. (BUT) With a cutoff of 35, about 43 percent of those tests would no longer qualify as positive. (AND) About 63 percent would no longer be judged positive if the cycles were limited to 30,”
“In Massachusetts, from 85 to 90 percent of people who tested positive in July with a cycle threshold of 40 would have been deemed negative if the threshold were 30 cycles…I would say that none of those people should be contact-traced, not one.” Said Dr. Michael Mina, an epidemiologist at the Harvard T.H. Chan School of Public Health
_________________________________
Some of the nation’s leading public health experts are raising a new concern in the endless debate over coronavirus testing in the United States: The standard tests are diagnosing huge numbers of people who may be carrying relatively insignificant amounts of the virus.
Most of these people are not likely to be contagious and identifying them may contribute to bottlenecks that prevent those who are contagious from being found in time. But researchers say the solution is not to test less, or to skip testing people without symptoms, as recently suggested by the Centers for Disease Control and Prevention.
Instead, new data underscore the need for more widespread use of rapid tests, even if they are less sensitive.
“The decision not to test asymptomatic people is just really backward,” said Dr. Michael Mina, an epidemiologist at the Harvard T.H. Chan School of Public Health, referring to the C.D.C. recommendation.
“In fact, we should be ramping up testing of all different people,” he said, “but we have to do it through whole different mechanisms.”
In what may be a step in this direction, the Trump administration announced on Thursday that it would purchase 150 million rapid tests.
The most widely used diagnostic test for the new coronavirus, called a PCR test, provides a simple yes-no answer to the question of whether a patient is infected.
But similar PCR tests for other viruses do offer some sense of how contagious an infected patient may be: The results may include a rough estimate of the amount of virus in the patient’s body. “We’ve been using one type of data for everything, and that is just plus or minus — that’s all,” Dr. Mina said. “We’re using that for clinical diagnostics, for public health, for policy decision-making.”
But yes/no isn’t good enough, he added. It’s the amount of virus that should dictate the infected patient’s next steps. “It’s really irresponsible, I think, to forgo the recognition that this is a quantitative issue,” Dr. Mina said
.
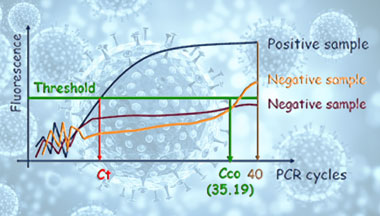
The PCR test amplifies genetic matter from the virus in cycles; the fewer cycles required, the greater the amount of virus, or viral load, in the sample. The greater the viral load, the more likely the patient is to be contagious.
This number of amplification cycles needed to find the virus, called the cycle threshold, is never included in the results sent to doctors and coronavirus patients, although it could tell them how infectious the patients are.
In three sets of testing data that include cycle thresholds, compiled by officials in Massachusetts, New York and Nevada, up to 90 percent of people testing positive carried barely any virus, a review by The Times found.
Coronavirus Briefing: An informed guide to the global outbreak, with the latest developments and expert advice.
On Thursday, the United States recorded 45,604 new coronavirus cases, according to a database maintained by The Times. If the rates of contagiousness in Massachusetts and New York were to apply nationwide, then perhaps only 4,500 of those people may actually need to isolate and submit to contact tracing.
One solution would be to adjust the cycle threshold used now to decide that a patient is infected. Most tests set the limit at 40, a few at 37. This means that you are positive for the coronavirus if the test process required up to 40 cycles, or 37, to detect the virus.
Tests with thresholds so high may detect not just live virus but also genetic fragments, leftovers from infection that pose no particular risk — akin to finding a hair in a room long after a person has left, Dr. Mina said.
“Any test with a cycle threshold above 35 is too sensitive”, agreed Juliet Morrison, a virologist at the University of California, Riverside. “I’m shocked that people would think that 40 could represent a positive,” she said.
“A more reasonable cutoff would be 30 to 35”, she added. Dr. Mina said he would set the figure at 30, or even less. Those changes would mean the amount of genetic material in a patient’s sample would have to be 100-fold to 1,000-fold that of the current standard for the test to return a positive result — at least, one worth acting on.
“It’s just kind of mind-blowing to me that people are not recording the Ct values from all these tests, that they’re just returning a positive or a negative,” one virologist said.
The Food and Drug Administration said in an emailed statement that it does not specify the cycle threshold ranges used to determine who is positive, and that “commercial manufacturers and laboratories set their own.”
The Centers for Disease Control and Prevention said it is examining the use of cycle threshold measures “for policy decisions.” The agency said it would need to collaborate with the FDA and with device manufacturers to ensure the measures “can be used properly and with assurance that we know what they mean.”
The CDC’s own calculations suggest that it is extremely difficult to detect any live virus in a sample above a threshold of 33 cycles. Officials at some state labs said the CDC had not asked them to note threshold values or to share them with contact-tracing organizations.
For example, North Carolina’s state lab uses the Thermo Fisher coronavirus test, which automatically classifies results based on a cutoff of 37 cycles. A spokeswoman for the lab said testers did not have access to the precise numbers.
This amounts to an enormous, missed opportunity to learn more about the disease, some experts said.
“It’s just kind of mind-blowing to me that people are not recording the Ct values from all these tests — that they’re just returning a positive or a negative,” said Angela Rasmussen, a virologist at Columbia University in New York.
“It would be useful information to know if somebody’s positive, whether they have a high viral load or a low viral load,” she added.
Words to Know About Testing for Covid-19
Confused by the terms about coronavirus testing? Let us help:
Antibody: A protein produced by the immune systemthat can recognize and attach precisely to specific kinds of viruses, bacteria, or other invaders.
Antibody test/serology test: A test that detects antibodies specific to the coronavirus. Antibodies begin to appear in the blood about a week after the coronavirus has infected the body. Because antibodies take so long to develop, an antibody testcan’t reliably diagnose an ongoing infection.But it can identify people who have been exposed to the coronavirus in the past.
Antigen test: This test detects bits of coronavirus proteins called antigens. Antigen tests are fast, taking as little as five minutes, but are less accuratethan tests that detect genetic material from the virus.
Coronavirus: Any virus that belongs to the Orthocoronavirinae family of viruses. The coronavirus that causes Covid-19 is known as SARS-CoV-2.
Covid-19: The disease caused by the new coronavirus. The name is short for coronavirus disease 2019.
Isolation and quarantine: Isolation is the separation ofpeople who know they are sick with a contagious disease from those who are not sick.Quarantinerefers to restricting the movement of people who have been exposed to a virus.
Nasopharyngeal swab: A long, flexible stick, tipped with a soft swab, that is inserted deep into the nose to get samples from the space where the nasal cavity meets the throat. Samples for coronavirus tests can also be collected with swabs that do not go as deep into the nose—sometimes called nasal swabs —or oral or throat swabs.
Polymerase Chain Reaction (PCR): Scientists use PCR to make millions of copies of genetic material in a sample. Tests that use PCR enable researchers to detect the coronavirus even when it is scarce.
Viral load: The amount of virus in a person’s body. In people infected by the coronavirus, the viral load may peak before they start to show symptoms,if symptoms appear at all.
Officials at the Wadsworth Center, New York’s state lab, have access to Ct values from tests they have processed, and analyzed their numbers at The Times’s request. In July, the lab identified 872 positive tests, based on a threshold of 40 cycles.
With a cutoff of 35, about 43 percent of those tests would no longer qualify as positive. About 63 percent would no longer be judged positive if the cycles were limited to 30.
In Massachusetts, from 85 to 90 percent of people who tested positive in July with a cycle threshold of 40 would have been deemed negative if the threshold were 30 cycles, Dr. Mina said. “I would say that none of those people should be contact-traced, not one,” he said.
Other experts informed of these numbers were stunned.
“I’m really shocked that it could be that high — the proportion of people with high Ct value results,” said Dr. Ashish Jha, director of the Harvard Global Health Institute. “Boy, does it really change the way we need to be thinking about testing.”
Dr. Jha said he had thought of the PCR test as a problem because it cannot scale to the volume, frequency or speed of tests needed. “But what I am realizing is that a really substantial part of the problem is that we’re not even testing the people who we need to be testing,” he said.
“The number of people with positive results who aren’t infectious is particularly concerning,” said Scott Becker, executive director of the Association of Public Health Laboratories. “That worries me a lot, just because it’s so high,” he said, adding that the organization intended to meet with Dr. Mina to discuss the issue.
The FDA noted that people may have a low viral load when they are newly infected. A test with less sensitivity would miss these infections.
But that problem is easily solved, Dr. Mina said: “Test them again, six hours later or 15 hours later or whatever,” he said. A rapid test would find these patients quickly, even if it were less sensitive, because their viral loads would quickly rise.
PCR tests still have a role, he and other experts said. For example, their sensitivity is an asset when identifying newly infected people to enroll in clinical trials of drugs.
But with 20 percent or more of people testing positive for the virus in some parts of the country, Dr. Mina and other researchers are questioning the use of PCR tests as a frontline diagnostic tool.
People infected with the virus are most infectious from a day or two before symptoms appear till about five days after. But at the current testing rates, “you’re not going to be doing it frequently enough to have any chance of really capturing somebody in that window,” Dr. Mina added.
Highly sensitive PCR tests seemed like the best option for tracking the coronavirus at the start of the pandemic. But for the outbreaks raging now, he said, what’s needed are coronavirus tests that are fast, cheap and abundant enough to frequently test everyone who needs it — even if the tests are less sensitive.
“It might not catch every last one of the transmitting people, but it surely will catch the most transmissible people, including the (so-called) super-spreaders,” Dr. Mina said. “That alone would drive epidemics practically to zero.”
*Apoorva Mandavilli is a reporter focusing on science and global health. She is the 2019 winner of the Victor Cohn Prize for Excellence in Medical Science Reporting. @apoorva_nyc
-###-
Dr Gary G. Kohls lives in the USA and writes a weekly column, entitled Duty to Warn, for the Duluth Reader, Duluth, Minnesota’s alternative newsweekly magazine. His columns deal with the dangers of American Friendly Fascism, corporatism, Oligarchy, militarism, racism, malnutrition, and Big Pharma’s over-drugging and over-vaccinating agendas as well as other movements that threaten the environment, democracy, civility, health and the sustainability and livability of the planet and the future of the children.
Dr. Kohls is a past member of Mind Freedom International, the International Center for the Study of Psychiatry and Psychology and the International Society for Traumatic Stress Studies and is a signatory to and/or an advocate of the principles of the Great Barrington Declaration, the World Doctors Alliance and Americas Front Line Doctors. His practice of holistic medicine mainly involved helping the survivors of psychiatry that had often been mis-diagnosed, over-diagnosed and always over-medicated with un-approved and un-tested-for-safety cocktails of neurotoxic psychiatric drugs that not only had sickened them but to which they had also become addicted.
His Duty to Warn columns have been re-published around the world for the last decade. They deal frequently also deal with Big Vaccine’s over-vaccinating, Big Medicine’s over-screening, over-diagnosing and over-treating agendas
Many of Dr Kohls’ columns have been archived at a number of websites, including: http://duluthreader.com/search?search_term=Duty+to+Warn&p=2; http://www.globalresearch.ca/author/gary-g-kohls; http://freepress.org/geographic-scope/national; https://www.lewrockwell.com/author/gary-g-kohls/?ptype=article; and https://www.transcend.org/tms/author/?a=Gary%20G.%20Kohls,%20MD